Arthritis affects millions of people worldwide, causing joint pain, stiffness, and reduced mobility. It is not a single disease but a group of over 100 conditions that affect the joints and surrounding tissues. The most common forms are osteoarthritis (OA) and rheumatoid arthritis (RA).
Many people dismiss early joint pain as a natural part of aging. However, medical research shows that early diagnosis and treatment of arthritis can dramatically slow disease progression, preserve joint function, and improve the patient’s overall quality of life.
This article explores why early treatment helps, how to recognize early signs, and the best modern treatments and lifestyle strategies for managing arthritis effectively.
Table of Contents
1: Understanding Arthritis
1.1 What Is Arthritis?
Arthritis literally means “inflammation of the joints.” It can affect one or multiple joints, leading to pain, swelling, and stiffness.
The two major types are:
-
Osteoarthritis (OA): Caused by wear and tear of cartilage — the smooth tissue that cushions joints. It usually affects knees, hips, and hands.
-
Rheumatoid Arthritis (RA): An autoimmune disease in which the immune system mistakenly attacks joint tissues, leading to inflammation and eventual joint damage.
Other forms include psoriatic arthritis, gout, lupus-related arthritis, and juvenile arthritis.
1.2 Causes and Risk Factors
Common risk factors include:
-
Age (especially over 40 for OA)
-
Family history of arthritis
-
Obesity (extra weight adds stress to joints)
-
Previous joint injuries
-
Autoimmune disorders
-
Gender (women are more likely to develop RA)
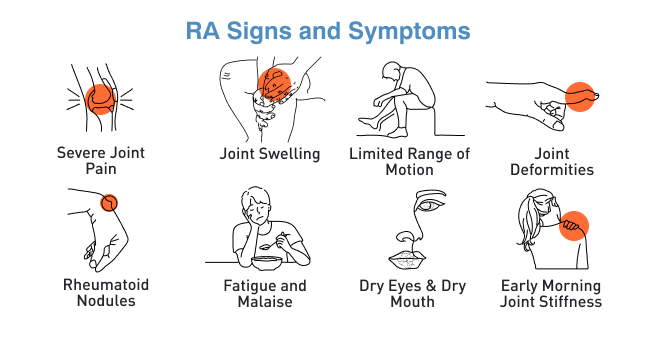
1.3 Symptoms to Watch For
Early signs may include:
-
Persistent joint pain
-
Morning stiffness lasting more than 30 minutes
-
Redness or swelling around joints
-
Fatigue or low-grade fever (especially in autoimmune arthritis)
-
Limited range of motion
Recognizing these symptoms early can lead to faster diagnosis and better long-term outcomes.
2: The Importance of Early Diagnosis
2.1 Early Detection Prevents Joint Damage
When arthritis goes untreated, chronic inflammation gradually erodes the cartilage and bone. Once this damage occurs, it cannot be reversed. Early intervention can slow or even halt this destructive process, preserving joint function.
2.2 Improved Treatment Outcomes
Starting treatment in the early stages often means:
-
Fewer medications needed later
-
Lower doses of painkillers
-
Better response to physical therapy
-
Reduced risk of deformity
For autoimmune arthritis like RA, early use of disease-modifying antirheumatic drugs (DMARDs) can prevent long-term disability.
2.3 Diagnosis Process
Doctors may use:
-
Physical examination: Checking for joint swelling, tenderness, and flexibility
-
Blood tests: To detect inflammation markers (ESR, CRP) or autoantibodies (RF, anti-CCP)
-
X-rays or MRI scans: To detect early cartilage or bone changes
3: Medical Treatments for Arthritis
3.1 Medications
-
NSAIDs (Nonsteroidal Anti-inflammatory Drugs):
Such as ibuprofen or naproxen to reduce pain and inflammation. -
Corticosteroids:
Powerful anti-inflammatories for short-term relief. -
DMARDs (Disease-Modifying Antirheumatic Drugs):
For autoimmune arthritis (e.g., methotrexate, hydroxychloroquine). -
Biologic Response Modifiers:
Target specific immune system components (e.g., adalimumab, etanercept). -
Analgesics:
Pain relievers like acetaminophen for mild symptoms.
3.2 Physical and Occupational Therapy
-
Physiotherapy: Improves mobility, muscle strength, and joint stability.
-
Occupational therapy: Helps patients adapt their daily activities to reduce strain.
-
Assistive devices: Braces, canes, or ergonomic tools help ease joint pressure.
3.3 Surgical Options
When conservative treatments fail, surgery may help:
-
Arthroscopy: Removes damaged cartilage or bone fragments.
-
Joint replacement (Arthroplasty): Replaces the damaged joint with an artificial one.
-
Joint fusion: Used for smaller joints to relieve pain.
4: Lifestyle and Home Remedies
4.1 Diet and Nutrition
Certain foods can help reduce inflammation and improve joint health:
-
Omega-3 fatty acids: Found in salmon, flaxseeds, and walnuts.
-
Antioxidants: Berries, spinach, and green tea.
-
Vitamin D and Calcium: Strengthen bones and prevent osteoporosis.
-
Turmeric (Curcumin): Natural anti-inflammatory.
Avoid processed foods, sugary snacks, and excess red meat as they can worsen inflammation.
4.2 Exercise and Physical Activity
Low-impact exercises help maintain flexibility and strength:
-
Walking
-
Swimming
-
Cycling
-
Yoga and stretching
Exercise improves joint lubrication, reduces stiffness, and supports weight control.
4.3 Weight Management
Excess weight places added stress on weight-bearing joints like knees and hips. Losing even a few kilograms can dramatically reduce pain and slow disease progression.
4.4 Stress Reduction
Chronic stress can worsen inflammation. Techniques like meditation, deep breathing, and mindfulness can enhance both mental and physical health.
5: Modern Advances in Arthritis Treatment
5.1 Biologic Therapies
Biologics are a breakthrough in arthritis care. They specifically target molecules involved in inflammation, offering personalized treatment with fewer side effects.
5.2 Regenerative Medicine
Research in stem cell therapy and platelet-rich plasma (PRP) aims to repair damaged cartilage and reduce inflammation.
5.3 Digital Health & Remote Monitoring
Mobile apps and wearable devices now track symptoms, medication schedules, and physical activity, helping doctors fine-tune treatment plans remotely.
6: Preventing Arthritis Progression
6.1 Early Screening
If you have a family history or early symptoms, consult a rheumatologist early for screening.
6.2 Stay Active
Regular movement keeps joints flexible. Even gentle stretches can prevent stiffness.
6.3 Balanced Diet and Hydration
Proper hydration keeps cartilage healthy, while a nutrient-rich diet supports bone density.
6.4 Avoid Joint Overuse
Alternate activities, take breaks, and use proper posture to protect your joints.
7: Living Positively with Arthritis
A diagnosis of arthritis doesn’t have to mean a lifetime of pain. With early treatment, patients can lead full, active lives.
Tips for Coping Emotionally:
-
Join arthritis support groups
-
Learn relaxation techniques
-
Celebrate small improvements
-
Focus on abilities, not limitations
With the right approach, arthritis becomes a manageable condition, not a defining one.
Read More – Dr. Harshna Bijlani: The Leading Aesthetic Dermatologist and Skin Expert in Mumbai
Conclusion: The Power of Early Action
Early treatment of arthritis is not just about managing pain — it’s about protecting your future mobility and independence. The sooner arthritis is diagnosed and treated, the greater the chances of preventing irreversible joint damage.
Consulting a doctor at the first sign of joint pain could make the difference between a life of mobility and one limited by stiffness and pain.
Remember: Don’t wait for arthritis to control your life — take control early.
FAQs About Arthritis Early Treatment
1. What is the best time to start arthritis treatment?
As soon as you notice persistent joint pain or stiffness lasting more than two weeks, consult a doctor. Early intervention provides the best outcomes.
2. Can arthritis be cured completely?
There’s no complete cure yet, but early treatment can effectively control symptoms and prevent joint damage.
3. Does diet affect arthritis?
Yes. Anti-inflammatory foods like fish, berries, and leafy greens can help, while processed foods can worsen symptoms.
4. Is exercise safe for arthritis patients?
Yes, gentle exercises like swimming, yoga, and walking are beneficial. Avoid high-impact activities that strain joints.
5. What are the warning signs of rheumatoid arthritis?
Early symptoms include morning stiffness, swelling in small joints (hands, feet), fatigue, and low-grade fever.
6. Which doctor should I see for arthritis?
A rheumatologist specializes in diagnosing and treating arthritis and related autoimmune diseases.
7. Can stress make arthritis worse?
Yes. Stress increases inflammatory responses in the body. Relaxation and mindfulness can help manage symptoms.
8. What are the latest arthritis treatments available?
Biologics, DMARDs, and regenerative medicine (like PRP and stem cell therapy) are cutting-edge options for arthritis management.